¹Licenciada en Nutrición. Especialista en Nutrición Pediátrica. Magíster en Nutrición y Biotecnología Alimentaria. Nutricionista del Servicio de Neonatología, Hospital J.B. Iturraspe, Santa Fe, Argentina. Docente de la Universidad Católica de Santa Fe, Argentina. ORCID: 0000-0002-8169-2744
Correspondencia: nutjesicadiaz@gmail.com
Conflicto de intereses: Ninguno que declarar.
Recibido: 14 de febrero de 2024
Aceptado: 2 de abril de 2024
REFERENCIAS
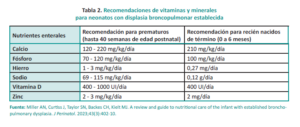
1. Miller AN, Curtiss J, Taylor SN, Backes CH, Kielt MJ. A review and guide to nutritional care of the infant with established bronchopulmonary dysplasia. J Perinatol. 2023;43(3):402-410.
2. Poindexter BB, Martin CR. Impact of Nutrition on Bronchopulmonary Dysplasia. Clin Perinatol. 2015;42(4):797-806.
3. Arigliani M, Spinelli AM, Liguoro I, Cogo P. Nutrition and Lung Growth. Nutrients. 2018;10(7):919.
4. Moya F. Preterm nutrition and the lung. World Rev Nutr Diet. 2014;110:239-52.
5. Piersigilli F, Van Grambezen B, Hocq C, Danhaive O. Nutrients and Microbiota in Lung Diseases of Prematurity: The Placenta-Gut-Lung Triangle. Nutrients. 2020;12(2):469.
6. Ma L, Zhou P, Neu J, Lin HC. Potential Nutrients for Preventing or Treating Bronchopulmonary Dysplasia. Paediatr Respir Rev. 2017;22:83-88.
7. Natarajan G, Johnson YR, Brozanski B, Farrow KN, Zaniletti I, Padula MA, et al. Postnatal Weight Gain in Preterm Infants with Severe Bronchopulmonary Dysplasia. Am J Perinatol. 2014;31(3):223-30.
8. Northway WH Jr, Moss RB, Carlisle KB, Parker BR, et al. Late pulmonary sequelae of bronchopulmonary dysplasia. N Engl J Med. 1990;323(26):1793-9.
9. Mataloun MM, Leone CR, Mascaretti RS, Dohlnikoff M, Rebello CM. Effect of postnatal malnutrition on hyperoxia-induced newborn lung development. Braz J Med Biol Res. 2009;42(7):606-13.
10. Frank L, Sosenko IR. Undernutrition as a major contributing factor in the pathogenesis of bronchopulmonary dysplasia. Am Rev Respir Dis. 1988;138(3):725-9.
11. Abman SH, Collaco JM, Shepherd EG, Keszler M, et al. Interdisciplinary Care of Children with Severe Bronchopulmonary Dysplasia. J Pediatr. 2017;181:12-28.e1.
12. Jensen EA, Dysart K, Gantz MG, McDonald S, et al. The Diagnosis of Bronchopulmonary Dysplasia in Very Preterm Infants. An Evidence-based Approach. Am J Respir Crit Care Med. 2019;200(6):751-759.
13. Barrington KJ, Fortin‐Pellerin E, Pennaforte T. Fluid restriction for treatment of preterm infants with chronic lung disease. Cochrane Database Syst Rev. 2017;2017(2):CD005389.
14. Uberos J, Jimenez-Montilla S, Molina-Oya M, García-Serrano JL. Early energy restriction in premature infants and bronchopulmonary dysplasia: a cohort study. Br J Nutr. 2020;123(9):1024-1031.
15. Principi N, Di Pietro GM, Esposito S. Bronchopulmonary dysplasia: clinical aspects and preventive and therapeutic strategies. J Transl Med. 2018;16(1):36.
16. Roberts K, Stepanovich G, Bhatt-Mehta V, Donn SM. New Pharmacologic Approaches to Bronchopulmonary Dysplasia. J Exp Pharmacol. 2021;13:377-396.
17. Wassner SJ. Altered growth and protein turnover in rats fed sodium-deficient diets. Pediatr Res. 1989;26(6):608-13.
18. Curtiss J, Zhang H, Griffiths P, Shepherd EG, Lynch S. Nutritional Management of the Infant With Severe Bronchopulmonary Dysplasia. NeoReviews. 2015;16(12):e674-e679.
19. Park JS, Jeong SA, Cho JY, Seo JH, et al. Risk Factors and Effects of Severe Late-Onset Hyponatremia on Long-Term Growth of Prematurely Born Infants. Pediatr Gastroenterol Hepatol Nutr. 2020;23(5):472-483.
20. Hansmann G, Sallmon H, Roehr CC, Kourembanas S, et al. Pulmonary hypertension in bronchopulmonary dysplasia. Pediatr Res. 2021;89(3):446-455.
21. Bamat NA, Kirpalani H, Feudtner C, Jensen EA, et al. Medication use in infants with severe bronchopulmonary dysplasia admitted to United States children’s hospitals. J Perinatol. 2019;39(9):1291-1299.
22. Kielt MJ, Logan JW, Backes CH, Conroy S, et al. Noninvasive Respiratory Severity Indices Predict Adverse Outcomes in Bronchopulmonary Dysplasia. J Pediatr. 2022;242:129-136.e2.
23. Lewis T, Truog W, Nelin L, Napolitano N, McKinney RL. Pharmacoepidemiology of Drug Exposure in Intubated and Non-Intubated Preterm Infants With Severe Bronchopulmonary Dysplasia. Front Pharmacol. 2021;12:695270.
24. Leitch CA, Ahlrichs J, Karn C, Denne SC. Energy Expenditure and Energy Intake During Dexamethasone Therapy for Chronic Lung Disease. Pediatr Res. 1999;46(1):109-13.
25. Van Goudoever JB, Wattimena JD, Carnielli VP, Sulkers EJ, et al. Effect of dexamethasone on protein metabolism in infants with bronchopulmonary dysplasia. J Pediatr. 1994;124(1):112-8.
26. Appel B, Fried SK. Effects of insulin and dexamethasone on lipoprotein lipase in human adipose tissue. Am J Physiol. 1992;262(5 Pt 1):E695-699.
27. Hauner H, Schmid P, Pfeiffer EF. Glucocorticoids and insulin promote the differentiation of human adipocyte precursor cells into fat cells. J Clin Endocrinol Metab. 1987;64(4):832-5.
28. Bauer SE, Huff KA, Vanderpool CPB, Rose RS, Cristea AI. Growth and nutrition in children with established bronchopulmonary dysplasia: A review of the literature. Nutr Clin Pract. 2022;37(2):282-298.
29. Wang LY, Luo HJ, Hsieh WS, Hsu CH, et al. Severity of bronchopulmonary dysplasia and increased risk of feeding desaturation and growth delay in very low birth weight preterm infants. Pediatr Pulmonol. 2010;45(2):165-73.
30. Malkar MB, Gardner W, Welty SE, Jadcherla SR. Antecedent Predictors of Feeding Outcomes in Premature Infants With Protracted Mechanical Ventilation. J Pediatr Gastroenterol Nutr. 2015;61(5):591-5.
31. Hatch LD, Scott TA, Walsh WF, Goldin AB, et al. National and Regional Trends in Gastrostomy in Very Low Birth Weight Infants in the US: 2000-2012. J Perinatol. 2018;38(9):1270-1276.
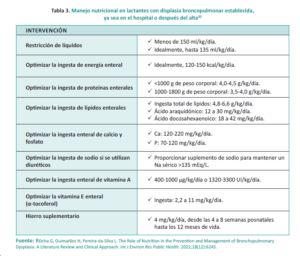
32. Rocha G, Guimarães H, Pereira-da-Silva L. The Role of Nutrition in the Prevention and Management of Bronchopulmonary Dysplasia: A Literature Review and Clinical Approach. Int J Environ Res Public Health. 2021;18(12):6245.
33. Bozzetti V, De Angelis C, Tagliabue PE. Nutritional approach to preterm infants on noninvasive ventilation: An update. Nutrition. 2017;37:14-17.
34, Oh W. Fluid and electrolyte management of very low birth weight infants. Pediatr Neonatol. 2012;53(6):329-33.
35. Sweet DG, Carnielli V, Greisen G, Hallman M, et al. European Consensus Guidelines on the Management of Respiratory Distress Syndrome – 2019 Update. Neonatology. 2019;115(4):432-450.
36. Bell EF, Warburton D, Stonestreet BS, Oh W. Effect of fluid administration on the development of symptomatic patent ductus arteriosus and congestive heart failure in premature infants. N Engl J Med. 1980;302(11):598-604.
37. Guo MM, Chung CH, Chen FS, Chen CC, et al. Severe bronchopulmonary dysplasia is associated with higher fluid intake in very low-birth-weight infants: a retrospective study. Am J Perinatol. f 2015;30(2):155-62.
38. Zhang R, Lin XZ, Chang YM, Liu XH, et al. [Expert consensus on nutritional management of preterm infants with bronchopulmonary dysplasia]. Zhongguo Dang Dai Er Ke Za Zhi. 2020;22(8):805-814. Chinese.
39. Stokowski LA. Fundamentals of phototherapy for neonatal jaundice. Adv Neonatal Care. 2006;6(6):303-12.
40. Bose C, Van Marter LJ, Laughon M, O’Shea TM, et al. Fetal growth restriction and chronic lung disease among infants born before the 28th week of gestation. Pediatrics. 2009;124(3):e450-458.
41. Biniwale MA, Ehrenkranz RA. The role of nutrition in the prevention and management of bronchopulmonary dysplasia. Semin Perinatol. 2006;30(4):200-8.
42. Denne SC. Energy expenditure in infants with pulmonary insufficiency: is there evidence for increased energy needs? J Nutr. 2001;131(3):935S-937S.
43. de Meer K, Westerterp KR, Houwen RH, Brouwers HA, et al. Total energy expenditure in infants with bronchopulmonary dysplasia is associated with respiratory status. Eur J Pediatr. 1997;156(4):299-304.
44. Groothuis JR, Makari D. Definition and outpatient management of the very low-birth-weight infant with bronchopulmonary dysplasia. Adv Ther. 2012;29(4):297-311.
45. Agostoni C, Buonocore G, Carnielli VP, De Curtis M, et al. Enteral nutrient supply for preterm infants: commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2010;50(1):85-91.
46. Fenton TR, Groh-Wargo S, Gura K, Martin CR, et al. Effect of Enteral Protein Amount on Growth and Health Outcomes in Very-Low-Birth-Weight Preterm Infants: Phase II of the Pre-B Project and an Evidence Analysis Center Systematic Review. J Acad Nutr Diet. 2021;121(11):2287-2300.e12.
47. Thomas N. Nutritional care of preterm infants: Scientific basis and practical guidelines. Indian J Med Res. 2016;143(4):531-532.
48. Massaro D, Massaro GD. Retinoids, alveolus formation, and alveolar deficiency: clinical implications. Am J Respir Cell Mol Biol. 2003;28(3):271-4.
49. Mandell E, Seedorf G, Gien J, Abman SH. Vitamin D treatment improves survival and infant lung structure after intra-amniotic endotoxin exposure in rats: potential role for the prevention of bronchopulmonary dysplasia. Am J Physiol Lung Cell Mol Physiol. 2014;306(5):L420-428.
50. Lee GY, Han SN. The Role of Vitamin E in Immunity. Nutrients. 2018;10(11):1614.
51. Falciglia HS, Johnson JR, Sullivan J, Hall CF, et al. Role of antioxidant nutrients and lipid peroxidation in premature infants with respiratory distress syndrome and bronchopulmonary dysplasia. Am J Perinatol. 2003;20(2):97-107.
52. Ehrenkranz RA, Ablow RC, Warshaw JB. Effect of vitamin E on the development of oxygen-induced lung injury in neonates. Ann N Y Acad Sci. 1982;393:452-66.
53. Terrin G, Berni Canani R, Di Chiara M, Pietravalle A, et al. Zinc in Early Life: A Key Element in the Fetus and Preterm Neonate. Nutrients. 2015;7(12):10427-46.
54. Vázquez-Gomis R, Bosch-Gimenez V, Juste-Ruiz M, Vázquez-Gomis C, et al. Zinc concentration in preterm newborns at term age, a prospective observational study. BMJ Paediatr Open. 2019;3(1):e000527.
55. Shaikhkhalil AK, Curtiss J, Puthoff TD, Valentine CJ. Enteral zinc supplementation and growth in extremely-low-birth-weight infants with chronic lung disease. J Pediatr Gastroenterol Nutr. 2014;58(2):183-7.
56. Cohen N, Golik A. Zinc balance and medications commonly used in the management of heart failure. Heart Fail Rev. 2006;11(1):19-24.
57. Miller AN, Curtiss J, Kielt MJ. Nutritional Needs of the Infant with Bronchopulmonary Dysplasia. NeoReviews. 2024;25(1):e12-e24.
58. Tindell R, Tipple T. Selenium: implications for outcomes in extremely preterm infants. J Perinatol. 2018;38(3):197-202.
59. Logan JW, Lynch SK, Curtiss J, Shepherd EG. Clinical phenotypes and management concepts for severe, established bronchopulmonary dysplasia. Paediatr Respir Rev. 2019;31:58-63.
60. Miller AN, Moise AA, Cottrell L, Loomis K, et al. Linear growth is associated with successful respiratory support weaning in infants with bronchopulmonary dysplasia. J Perinatol. 2022;42(4):544-5.
61. Sanchez-Solis M, Perez-Fernandez V, Bosch-Gimenez V, Quesada JJ, Garcia-Marcos L. Lung function gain in preterm infants with and without bronchopulmonary dysplasia. Pediatr Pulmonol. 2016;51(9):936-42.
62. Huang J, Zheng Z, Zhao XY, Huang LH, et al. Short-term effects of fresh mother’s own milk in very preterm infants. Matern Child Nutr. 2023;19(1):e13430.
63. Xu Y, Yu Z, Li Q, Zhou J, et al. Dose-dependent effect of human milk on Bronchopulmonary dysplasia in very low birth weight infants. BMC Pediatr. 2020;20(1):522.
64. Kim LY, McGrath-Morrow SA, Collaco JM. Impact of breast milk on respiratory outcomes in infants with bronchopulmonary dysplasia. Pediatr Pulmonol. 2019;54(3):313-8.
65. Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2012;129(3):e827-841.
66. Morgan JA, Young L, McCormick FM, McGuire W. Promoting growth for preterm infants following hospital discharge. Arch Dis Child Fetal Neonatal Ed. 2012;97(4):F295-298.
67. Anderson C, Hillman NH. Bronchopulmonary Dysplasia: When the Very Preterm Baby Comes Home. Mo Med. 2019;116(2):117-22.
68. Botrán M, López-Herce J, Mencía S, Urbano J, et al. Enteral nutrition in the critically ill child: comparison of standard and protein-enriched diets. J Pediatr. 2011;159(1):27-32.e1.
69. Ong C, Han WM, Wong JJ, Lee JH. Nutrition biomarkers and clinical outcomes in critically ill children: A critical appraisal of the literature. Clin Nutr. 2014;33(2):191-7.
70. Gaio P, Verlato G, Daverio M, Cavicchiolo ME, et al. Incidence of metabolic bone disease in preterm infants of birth weight <1250 g and in those suffering from bronchopulmonary dysplasia. Clin Nutr ESPEN. 2018;23:234-9.
71. Chen W, Zhang Z, Dai S, Xu L. Risk factors for metabolic bone disease among preterm infants less than 32 weeks gestation with Bronchopulmonary dysplasia. BMC Pediatr. 2021;21(1):235.
72. Chinoy A, Mughal MZ, Padidela R. Metabolic bone disease of prematurity: causes, recognition, prevention, treatment and long-term consequences. Arch Dis Child Fetal Neonatal Ed. 2019;104(5):F560-6.
73. Abrams SA; Committee on Nutrition. Calcium and vitamin d requirements of enterally fed preterm infants. Pediatrics. 2013;131(5):e1676-1683.
74. Wood CL, Wood AM, Harker C, Embleton ND. Bone mineral density and osteoporosis after preterm birth: the role of early life factors and nutrition. Int J Endocrinol. 2013;2013:902513.
75. Pravia CI, Benny M. Long-term consequences of prematurity. Cleve Clin J Med. 2020;87(12):759-67.